|
Forums33
Topics44,197
Posts519,915
Members14,168
| |
Most Online3,221
Oct 6th, 2025
|
|
Administrator/owner:
John (Dragonslayer)
Administrator:
Melinda (mig)
WebAdmin:
Timo (Timo)
Administrator:
Brad (wolverinefan)
Moderators:
· Tim (Dotyisle)
· Chelsea (Kiwi)
· Megan (Megan)
· Wendy (WendyR)
· John (Cheerful)
· Chris (fyrfytr187)
|
|
If you want to use this QR code (Quick Response code) just save the image and paste it where you want. You can even print it and use it that way. Coffee cups, T-Shirts etc would all be good for the QR code.
|
|
|
|
Joined: Feb 2010
Posts: 96
Apprentice_AS_Kicker
|
OP

Apprentice_AS_Kicker
Joined: Feb 2010
Posts: 96 |
Having a bad flare on either side of my sternum, hurts to touch. I am currently doing the ice pack treatment. A friend of mine who is a pt told me to go cold shower then hot shower and ice after, that helps for about 30 minutes. Any other ideas, tricks or tips?
Pride makes us artificial and humility makes us real.
Thomas Merton
|
|
|
|
|
Joined: Jan 2008
Posts: 21,346 Likes: 2
Very_Addicted_to_AS_Kickin
|

Very_Addicted_to_AS_Kickin
Joined: Jan 2008
Posts: 21,346 Likes: 2 |
i just did a lot of ice. but contrasting ice and heat back and forth works even better for a lot of things, but is more work, so often i just use ice. also for me, the pain in the front where the ribs attached to the sternum seemed to be caused by rib issues in the back along the spine. by treating the ribs at the spine, helped the front too. last fall i noticed that swinging my arms when i walked made my costochondritis worse, so i walked with my hands in my pockets til it calmed down. can't really explain it, but noticed it. i also have some topical triple nsaid creme (kip gel) made by the local compounding pharmacist that helps if i have an acute spot. sorry you are having this pain. 
sue
Spondyloarthropathy, HLAB27 negative
Humira (still methylprednisone for flares, just not as often. Aleve if needed, rarely.)
LDN/zanaflex/flector patches over SI/ice
vits C, D. probiotics. hyaluronic acid. CoQ, Mg, Ca, K.
chiro
walk, bike
no dairy (casein sensitivity), limited eggs, limited yeast (bread)
|
|
|
|
|
Joined: Apr 2011
Posts: 34
Member
|

Member
Joined: Apr 2011
Posts: 34 |
Hi Sue
You say USpA...not diagnosed AS yet? What is USpA like? Why is it difficult to clinch the diagnosis?
|
|
|
|
|
Joined: Jan 2008
Posts: 21,346 Likes: 2
Very_Addicted_to_AS_Kickin
|

Very_Addicted_to_AS_Kickin
Joined: Jan 2008
Posts: 21,346 Likes: 2 |
hi disk, i think different people / different doctors define USpA differently. i know how my rheumatologist defines it because he wrote the WebMD description!  http://emedicine.medscape.com/article/332945-overview http://emedicine.medscape.com/article/332945-overviewUndifferentiated spondyloarthropathy:[18, 31]
Undifferentiated spondyloarthropathy is a syndrome with features consistent with the spondyloarthropathies, but affected patients do not fulfill criteria for any specific spondyloarthropathy. Criteria are outlined in Table 2 at the end of this section.
Undifferentiated spondyloarthropathy may represent an early phase or incomplete form of ankylosing spondylitis or another spondyloarthropathy. In fact, several studies of undifferentiated spondyloarthropathy included many patients who probably should have been diagnosed with ankylosing spondylitis, reactive arthritis, or IBD-associated spondyloarthropathy, which made the clinical description very ambiguous. However, more recent data suggest that these patients may represent a distinct disease entity based on demographic and clinical criteria.
Although no specific criteria are identified, using modified Amor criteria can be helpful in confirming a clinical diagnosis.[19]
Distinguishing features of undifferentiated spondyloarthropathy:[19]
The age of onset has a very wide range, with the peak onset at approximately age 50 years. The male-to-female ratio is 1:3. The onset is usually insidious, and, even after years of active disease, sacroiliitis and spondylitis are either absent or appear very mild on routine radiography.
Clinical manifestations of undifferentiated spondyloarthropathy include inflammatory back pain (90%), buttock pain (80%), enthesitis (85%), peripheral arthritis (35%), dactylitis (17%), and fatigue (55%).
Extra-articular manifestations are uncommon, occurring in fewer than 10% of patients, and include acute anterior uveitis (1-2%), oral ulcers, rash, nonspecific IBD, pleuritis, and pericarditis.
Findings of laboratory studies are generally unremarkable except for the presence of an elevated ESR or C-reactive protein level (36%). HLA-B27 antigen is positive only in approximately 20-25% of patients.
These factors, especially the late age of onset, female predominance, and low HLA-B27 positivity, suggest that Undifferentiated spondyloarthropathy is distinct from ankylosing spondylitis and the other classic spondyloarthropathies.
In addition, when these patients are observed over long periods, they rarely develop clinical manifestations or radiographic changes that result in a change of diagnosis (outlined in Table 3, at the end of this section). Occasionally, radiographs show evidence of periosteal new bone formation at sites of enthesitis, especially at the insertion of the Achilles tendon or plantar fascia on the calcaneus, or early syndesmophytes on the lumbar spine without bridging.
Although most patients with undifferentiated spondyloarthropathy have chronic, active disease and require long-term therapy, some patients have mild and intermittent symptoms that require intermittent symptomatic therapy. These episodes may last from 1-2 weeks to several months, with long asymptomatic periods that do not require therapy.
Most patients with undifferentiated spondyloarthropathy (>75%) require long-term therapy for ongoing symptomatic disease. Most patients respond well to nonsteroidal anti-inflammatory drugs (NSAIDs). Most patients maintain good function without progressive disease or clinically significant radiographic changes. A small minority of patients does not respond well to or tolerate NSAIDs. In these patients, treatment progression is similar to patients with ankylosing spondylitis, including the use of sulfasalazine, methotrexate, and TNF-α antagonists, although no well-designed clinical trials have been conducted on the treatment of undifferentiated spondyloarthropathy.
Table 2. Diagnostic Criteria for Undifferentiated Spondyloarthropathy Using Modified Amor Criteria[32, 33] (Open Table in a new window)
Inclusion Criteria Exclusion Criteria
Inflammatory back pain 1 point Diagnosis of specific spondyloarthropathy
Unilateral buttock pain 1 point Sacroiliitis on radiograph ≥ grade 2
Alternating buttock pain 2 points Precipitating genitourinary/GI infection
Enthesitis 2 points Psoriasis
Peripheral arthritis 2 points Keratoderma blennorrhagicum
Dactylitis (sausage digit) 2 points IBD (Crohn disease or ulcerative colitis)
Acute anterior uveitis 2 points Positive rheumatoid factor
HLA-B27 –positive or family history of spondyloarthropathy 2 points Positive antinuclear antibody, titer >1:80
Good response to nonsteroidal anti-inflammatory drugs 2 points
Diagnosis of spondyloarthropathy with 6 or more points
Table 3. Clinical and Laboratory Features of Undifferentiated Spondyloarthropathy (Open Table in a new window)
Clinical Feature of Undifferentiated Spondyloarthropathy Frequency
Inflammatory back pain 90%
Buttock pain 80%
Enthesitis 75%
Peripheral arthritis 40%
Dactylitis (sausage digits) 20%
Acute anterior uveitis 1-2%
Fatigue 55%
Elevated ESR 32%
HLA-B27 –positive 25% the doctor came to undiff spondy because: i have "prominent" enthesitis (bad enough to tear tendons and ligaments), SI joint inflammation (diagnosed through symptoms, CT scan showing arthritic changes, cortisone injections and now flector patch being highly effective), and inflammation and ulcerations in my illeum (discovered by my gastroenterologist through a colonoscopy). also the fact that i've had dry eyes, mouth sores, and a few weird skin rashes, and that i respond to both nsaids and prednisone helped convince him. along with the morning stiffness and inflammation from being immobile (trouble with sitting too long, standing too long, laying too long). the doctor ruled out: 1. IBD (crohns and uc) (based on colonoscopy, CT enterography done through gastroenterologist) 2. psoriatic arthritis (skin involvement not significant enough) 3. AS (no evidence of fusing through scans, no uveitis / iritis, no HLAB27) the bottom line i came away with was that undiff spondy is "all the inflammation, none of the fusing." you ask, "what is USpA like?" i can only answer for myself. my main problems have been two fold. SI joint inflammation and all that goes along with that. and enthesitis bad enough to cause some pretty significant tendon and ligament tears over the years; not enough to cause a rupture, but enough so i lost use of my left hand for 2-3 years, or couldn't walk for almost a year; miraculously they healed with time. and what caused these things were as simple as pouring a pot of water into the sink or light stretching, not normal. though the last two years, my biggest problem has been my ribs, especially where they join at the spine. i also have primarily gastritis and secondarily IBS, i've been able to keep both mostly under control most of the time, but when not, the gastritis is very painful and the IBS causes me to not digest my food. my new rheumy thinks "all spondys start in the gut." (just quoting, no judgement here) for me that does seem to have been the case (GI issues 5 years before arthritis issues) so, not so much "not diagnosed with AS yet, but rather diagnosed with undifferentiated spondyloarthropathy". why is it difficult to clinch the diagnosis? i can only give my experience. i think it depended largely on the doctor i saw. most doctors were looking for evidence of fusing, elevated esr, elevated crp, ana for lupus, RF for RA. but this doctor understood how enthesitis does not necessarily lead to elevated crp or esr, and not everyone with a spondyloarthropathy fuses. this doctor also understood that the reason i was tearing tendons and ligaments was because i have a particularly bad case of enthesitis, when it flares that is. also, i flare and get better. if a doctor sees me in a better phase, it varies if they believe my descriptions of my flares or have to see it for themselves, a difference in philosophies. i used to think that having my husband there to validate my descriptions would help, but really it didn't seem to make much of a difference. the doctor in philadelphia (brent) and now my local rheumy, Dr P, have a better understanding of undiff spondy i think. plus they believe what i tell them and what my husband tells them, rather than having to see me at my worst. for me it was finding the right doctors. but now that i have, i can understand how hard it can be to diagnose undiff spondy. and to me the most important thing is that i have doctors who are helping me. their kindness is a nice plus.  thank you for asking. i hope my answers can help others who see themselves in my descriptions. anything that can shorten the time from onset to diagnosis.
Last edited by Sue22; 04/16/11 04:44 AM.
sue
Spondyloarthropathy, HLAB27 negative
Humira (still methylprednisone for flares, just not as often. Aleve if needed, rarely.)
LDN/zanaflex/flector patches over SI/ice
vits C, D. probiotics. hyaluronic acid. CoQ, Mg, Ca, K.
chiro
walk, bike
no dairy (casein sensitivity), limited eggs, limited yeast (bread)
|
|
|
|
|
Joined: Sep 2001
Posts: 2,469
Colonel_AS_Kicker
|

Colonel_AS_Kicker
Joined: Sep 2001
Posts: 2,469 |
Heat and Pennsaid works for me for some relief then I take tylenol 3 and relax to ride the flare out.
Dan
 >>>>>>  We are kicking some AS*.
|
|
|
|
|
Joined: Apr 2011
Posts: 34
Member
|

Member
Joined: Apr 2011
Posts: 34 |
sue, thank you so much...that is indeed great reference. lets see what the rheumy makes of all this...
|
|
|
|
|
Joined: Sep 2001
Posts: 6,179 Likes: 23
AS Czar
|

AS Czar
Joined: Sep 2001
Posts: 6,179 Likes: 23 |
Hi, sue:
I am sorry, but this hand-waiving is totally unconvincing, especially the part about...well, it is OK to have syndesmophytes in Udiff...ugh--as long as they are not BRIDGING SYNDESMOPHYTES..!!! That is just too illogical.
After reading this, I am MORE CONVINCED that Udiff is just another variety of AS. AS does not always cause such severe pains, and there are more people with AS who will end up fused and not know why (they never needed a diagnosis), but there is the other side of the same coin--plenty of people will have the pain, but never fuse. This is the part that is due to genetic variations; not "how many names can humans pin on a disease process of fusion by the nanometer?"
I suspected Crohn's and AS were just about the same disease, while I was observing a good friend with this disease, and I followed symptoms behind her by about two years. Well, it is the same CAUSE and mechanism on the Klebsiella-continuum; now I have added another one: I'm differentiated!
HEALTH,
John
|
|
|
|
|
Joined: Apr 2011
Posts: 34
Member
|

Member
Joined: Apr 2011
Posts: 34 |
why does chest expansion restriction start early on? if the fusing is not there why does it feel tough to pull in a breath? due to inflammation? so if the inflammation goes down with NSAIDS would the full breath come back? how should chest expansion be maintained and increased?
|
|
|
|
|
Joined: Jan 2008
Posts: 21,346 Likes: 2
Very_Addicted_to_AS_Kickin
|

Very_Addicted_to_AS_Kickin
Joined: Jan 2008
Posts: 21,346 Likes: 2 |
not completely sure where the disagreement is? you say undiff spondy, IBD are other forms of AS. the webMD says undiff spondy, AS, IBD, are different forms of spondyloarthropathy. the venn diagram shows large areas of overlap with AS in the middle. so rather than seeing the differences, i see the similarities. other than webMD calling them all spondyloarthropathies and you calling them all AS, i'm not sure how what you are saying and what webMD is saying as being a whole lot different. if i were to add my opinion, i'd say i couldn't disagree with either of you, i see more similarities than differences. 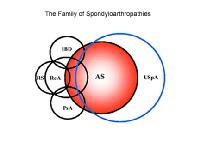 i'm going to pick up this conversation in another thread so this one can focus on costochondritis. want to share about my new in town rheumy.......
sue
Spondyloarthropathy, HLAB27 negative
Humira (still methylprednisone for flares, just not as often. Aleve if needed, rarely.)
LDN/zanaflex/flector patches over SI/ice
vits C, D. probiotics. hyaluronic acid. CoQ, Mg, Ca, K.
chiro
walk, bike
no dairy (casein sensitivity), limited eggs, limited yeast (bread)
|
|
|
|
|
Joined: Jan 2010
Posts: 2,105
Major_AS_Kicker
|

Major_AS_Kicker
Joined: Jan 2010
Posts: 2,105 |
Disk, I still don't have a diagnosis, have some changes on SI xray (sclerosis/erosions, but the radiologist says not typical of sacroiliitis) but have enormous problems with rib pain and very poor chest expansion (often only half an inch, and never more than an inch). I've also had the costochondritis type pains for many years along with the reduced chest expansion.
My way of dealing with it is to take NSAIDs at full therapeutic levels (its definitely worse if I don't take them), and I have also learned how to do deep tummy breathing (yoga breathing). I'm so good at getting a full lungful of air by doing the tummy breathing that when I first complained about chest wall pain and they did lung function tests they came back totally normal, in spite of the poor chest exansion. The only time I have real problems is when I get a cold/flu and a cough with it - I just can't cough well at all, so it does mean that gunk builds up in my lungs much easier and is much harder to get rid of. Luckily I don't get colds that often.
|
|
|
|
0 members (),
1,058
guests, and
105
robots. |
|
Key:
Admin,
Global Mod,
Mod
|
|
|
|